As one of the country’s leading cancer care consulting organizations, The Oncology Group provides comprehensive oncology program and business planning for cancer services growth and cancer center development. The Oncology Group’s planning model incorporates all aspects of the patient care continuum from early detection and screening through treatment and beyond. Our firm has the expertise and experience to provide an array of customized oncology consulting services for hospitals and physician practices.
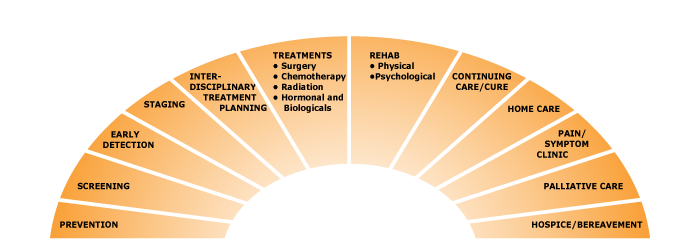
The Oncology Group’s planning model incorporates all aspects of the patient care continuum from early detection and screening through treatment and beyond. The Cancer Care Continuum, seen below, graphically represents this model.
What can we do to help you expand your cancer program?
Prevention
Establishing a cancer program’s expertise in cancer care occurs long before individuals are diagnosed with the disease. Complete community and academic programs consider themselves “go to” institutions for information from local experts about preventing cancer. Programs set up Resource Centers (including web access), provide clear clinical care links on their websites, provide community outreach education via Speaker’s Bureaus to address their cancer prevention missions, and often serve as sponsors for smoking cessation type initiatives.
The Oncology Group can assist your cancer care team members, notably physicians and clinical staff, to develop a community outreach plan for cancer prevention activities.
×Screening
Since early stage cancers are both more curable and elicit more favorable treatment outcomes, complete cancer programs offer a broad range of screening for site specific cancers with established tests – this includes mammography for breast cancer, PSA testing for prostate cancer, skin cancer visual screens, and PAP tests for cervical cancers. More invasive screens are available for colon cancer and other site-specific cancers.
TOG can assist your team to evaluate its volume and ROI for the cancer screening it supports, as well as to evaluate and assess interest in more specialized screening options such as broader use of low dose CT scans for lung cancer.
×Early Detection
Early detection goals are met through a combination of lifestyle education, screening services, and ease of access to specific diagnostic tests (e.g. mammography). Many programs couple with broad US initiatives that promote early detection of breast cancers, prostate cancers, and cervical cancers. Most states also provide financial support to ensure low-income or un/underinsured females can receive mammograms and PAP tests annually.
The Oncology Group is familiar with a broad array of local and national early detection initiatives, and can assist your team to evaluate its current early detection efforts, and to plan a 21st century early detection program, if needed.
×Staging
Anatomic staging, using the T(tumor), N(node), M (metastasis) nomenclature remains the foundation for prognostic classification of cancer. TNM staging is grounded on the foundation that a patient’s treatment options and survival opportunities reflect the extent of disease at presentation. TNC staging is aided by topographic site and histological type information. Furthermore, a great number of non-anatomic prognostic factors are currently in use or under study.
ACoS accreditation regulations require 90%+ of all cancer patient records include a stage assigned by the managing physician or another approved medical professional. The Oncology Group can assist your team to develop and implement a number of initiatives designed to increase your program’s compliance with this key accreditation standard.
×Interdisciplinary Treatment Planning
Numerous organizations (IOM, NCI) have reported that interdisciplinary treatment planning is a goal for cancer programs in the US. While most cancer programs describe their treatment planning process as multidisciplinary or interdisciplinary, more often, they are explaining a sequential cross-modality approach that involves more chart-writing (in medical records that are not shared across the entire treatment team) than meaningful discourse among physicians (and clinical staff) that yields an individual treatment “road map” for each specific patient. And the reality is individualized, real-time interdisciplinary treatment planning is a complicated endeavor, one not typically supported by existing infrastructure and certainly, not by private practice reimbursement models.
Because the ideal model is difficult to execute, The Oncology Group has developed a Play Book of successful (and less successful) organizations and efforts that have yielded practical interdisciplinary treatment planning forums. TOG can assist your team to evaluate your program’s current treatment planning model and to implement a more ideal and effective treatment planning approach.
×Treatments
• Surgery
• Chemotherapy
• Radiation
• Hormone & Biologicals
Cancer treatment includes the traditional three modalities of surgery, chemotherapy, and radiation oncology. Newer hormonal and biological treatments emerge frequently. The scope of services available to individual patients is critical in establishing a cancer program’s “comprehensiveness” and often, market recognition as a cancer center.
TOG provides a profile of treatment options your facility provides and assist in both the services which should be offered and the method to achieve national benchmarks for similar sized programs.
×Rehab
• Physical
• Psychological
The NCI notes, “It is natural for anyone who has completed cancer treatment to be concerned about what the future holds. Many people are concerned about the way they look and feel, and about what they can do to keep the cancer from recurring.” Several cancer programs are partnering with local physical fitness organizations or initiating their own physical and psychological rehab programs/services for their cancer patients who complete therapy and are working to resume a “new normal” life.
The Oncology Group can assist your team to develop budgets and investigate nationally-based programs that offer turn-key cancer rehabilitation services as part of your cancer services continuum.
×Continuing Care/Cure
The NCI estimates that there are over 12 million cancer survivors in the US today; this represents more than 4% of the US population. Furthermore, 67% of adults diagnosed with cancer will be alive in 5 years; among children, over 77% of childhood cancer survivors will be alive after 10 years. These individuals require long-term aftercare and surveillance. Many seek psycho-social assistance as they advance from cancer patient to cancer survivor. For adults who received cancer treatment as children, there is an increasingly recognized need to assess these individuals for late effects of their treatment.
The Oncology Group has much experience working with various US survivorship organizations. TOG is skilled in facilitating patient and survivor focus groups and can assist your team to develop a local or networked (with national and local organizations) Survivorship Program.
×Home Care
Most cancer care programs operate strong social work-based Home Care options for their patients. Patients are often more comfortable receiving care at home. However, this places important demands on family and friends, some of whom will assume caregiver roles.
×Pain/Symptom Clinic
Experts at the University of Illinois Chicago note that for more than 1.2 million Americans each year unrelieved cancer pain and fatigue are major health problems. Increasingly, cancer programs are developing pain management teams to address and treat pain, fatigue and other cancer treatment side-effects.
The Oncology Group can assist your team to create a Cancer Pain & Symptom Management Team in your institution.
×Palliative Care
Palliative Care addresses the emotional, physical, practical and spiritual issues of cancer. Palliative Care is sometimes offered not only to the patient, but also to family members. Palliative Care’s goal is to prevent or treat, as early as possible, the symptoms and side effects of cancer and/or its treatment. These issues can include psychological, social, and spiritual concerns. Palliative Care’s goal is not cure (though the patient may certainly continue receiving curative treatment in addition to palliative care). Palliative care is also called comfort care, supportive care, and symptom management.
TOG principals have long been leaders in the continually developing palliative care community. The Oncology Group can assist your team to develop a Palliative Care Plan and budget to implement an emerging, or a comprehensive Palliative Care Program or Team.
×Hospice/Bereavement
Hospice care is typically provided to a patient once cancer therapies are no longer controlling the disease. The focus of hospice services is caring, not disease treatment (cure). Typically, hospice patients have received a prognosis that they will live for 6 or fewer months, because of their disease progression.
Bereavement services are offered to cancer patients’ family and friends. During the bereavement period, individuals experience grief and mourn the loss of their friend or family member. Fatigue is also a recurring symptom for those grieving. Some cancer programs offer bereavement programs for young children of adult cancer patients.
×| Services | ||
|---|---|---|
| The following services are necessary to support each component of the continuum | ||
| Leadership/Infrastructure | Marketing | Counseling |
| Patient Support | Research | Transportation |
| Education and Information | Information Technology | Data Analysis |
| Accreditation(s) | Affiliation/Networking for Services | Accommodation |
Leadership/Infrastructure
Responsibility and accountability rely on conferred authority and individual leadership. Operationalizing a cancer program requires command and control responsibility coupled with interpersonal skills to plan and deliver program components that lie outside “traditional oncology care” department (e.g. diagnostic radiology).
The Oncology Group can assist your team to design a leadership and infrastructure model customized for your institution and cancer program.
Patient Support
Comprehensive cancer programs provide a score of patient services for which there are no billing codes, including pastoral care, support groups, and “I Can Cope” educational programs. Since these services are not billable, cancer programs must calculate budgets that include resources and staff to provide patients these necessary services.
The Oncology Group can assist your institution and cancer program leaders with inaugurating these “unbillable” but necessary patient and family care services; and with developing an inclusive cancer services budget.
Education and Information
Comprehensive cancer programs have a public position as cancer information providers. Smaller programs assume a responsibility for accurate public information about cancer prevention and early detection. Larger programs often assume responsibility, and provide a setting for, professional education about cancer care research and advances.
The Oncology Group can assist your team to inaugurate an episodic or annual public education calendar; or for academic affiliation institutions, TOG can assist the team to develop an annual professional education seminar or periodic grand rounds or tumor boards available to a regional professional audience.
×Accreditation(s)
For more than 75 years, the American College of Surgeons Commission on Cancer (ACoS-COC) has accredited cancer programs. Even smaller programs typically expect ACoS accreditation to mark their “official” entry into the ranks of US cancer programs. In the past decade, a number of organizations have also developed standards that enable leaders to validate their program’s quality. For example, NABPC offers accreditation for Breast Centers.
The Oncology Group’s staff has more than 60 years’ combined experience assisting institutions with obtaining initial ACoS accreditation. One of TOG’s consultants has been a leader in developing the NABPC Breast Center standards and accreditation process.
×Marketing
Successful cancer programs develop a marketing budget that enables the team to reach the public with information about its differentiating physicians, services, facilities, and seamless patient experience.
The Oncology Group is experienced in redirecting oncology marketing efforts away from “me too” or “we do this too” messages, to ensure key points of differentiation between your program and others in your market are highlighted. TOG is also experienced in working with cancer program leaders (including physicians) and the institution’s marketing department to develop an oncology-specific Marketing Plan and budget.
×Research
Research into cancer’s causes, cures, prevention, and care processes (patient experiences) remains a hallmark of complete cancer programs. While most programs struggle to meet ACoS requirements to enroll a minimum of 2% of their adult patients onto clinical trials, a number of community cancer programs exceed that rate, reaching adult enrollment of 10%+ their analytic cancer patient volume.
The Oncology Group can assist your team to expand its clinical trials programs, including broadening the physician base of those who place patients on trials, improving the enrollment process (including patient consent and IRB oversight) as well as expanding the number and variety of trials open.
×Information Technology
IT is a hallmark of integrated care that marks 21st century community cancer care delivery. IT has become one area that either differentiates a cancer program or is defined as one of the institution’s key weaknesses in delivering integrated care across a hospital and its affiliated private practice physicians. The ability of physicians to access, in real time, diagnostic studies and other modality physicians’ notes forms either a platform for multidisciplinary planning or a weakness in the program’s care delivery model.
×Affiliation/Networking for Services
Larger cancer programs can provide the majority of cancer care components, growing or smaller community programs cannot. And some elements (e.g. Phase I clinical research trials) are most often accessed in academic settings. Affiliation or cancer services networks provide one approach to ensuring local or regional patients have access, through your institution and physicians, to a full continuum of services – such as genetic testing, Proton beam therapy, site-specific surgeons, and similar specialty services.
The Oncology Group is experienced in working with hospital networks to “rationalize” cancer programs across several institutions, and with evaluating community hospital-Academic Medical Center affiliations’ opportunities and threats.
×Counseling
Cancer patients and their family members report their lives, from point of diagnosis and beyond (past initial treatment completion), are markedly stressful. Research data confirms patient compliance and patient satisfaction with their treatment, the cancer program institution, and their physicians is often sealed by the hands-on staff who counsel (formally or informally) throughout treatment. Counseling covers a variety of topics, from physical side-effects (e.g. mouthsores), to personal relations, to fear and anxiety. Patients identify counseling near the end of treatment as especially valuable.
The Oncology Group is well-versed in guiding teams across multiple disciplines some outside the traditional oncology service line, to develop psycho-social counseling plans for patients.
×Transportation
For a number of programs, notably those in clear urban and geographic rural locations, patient transportation to treatment sites is difficult. Radiation therapy is a daily exercise for five – seven weeks with patients often feeling weaker as the treatment ensues. Though chemotherapy is a a more episodic treatment modality, some patients still find it difficult to arrange transportation to the infusion center.
The Oncology Group can work with your social work team and outside agencies (e.g. The American Cancer Society) to develop transportation options.
×Data Analysis
Many hospitals that support cancer programs continue to rely on ICD-9 and inpatient volumes to assess the financial and “health & vitality” of their cancer programs. Data show ICD-9 computations woefully undercount cancer patient volume and revenue. It is vital to ensure hospital leaders understand cancer is primarily an outpatient service that drives not only oncology volumes, but diagnostic and pathology service volumes as well.
The Oncology Group is a leader in cancer program data analysis and application of this data to cancer program planning. Our data information provides cancer program physicians, and hospital leaders with information on site-specific cancer patient volume, oncology’s contribution to margin, referring physician volumes, institutional trends in geographic reach, and much valuable data on which firm growth and development plans depend.
×Accommodation
Cancer programs which offer specialty services, such as bone marrow transplant, and programs that serve a geographically dispersed region or have a regional destination program (e.g. the only radiation therapy service within 50+ miles) often find it important to develop hospitality industry relationships. These hotel-hospital accommodation agreements enable the patient, family and friends to stay near the cancer center, to ensure treatment continues daily and to do so within the constraints of a family budget. Some AMC programs have introduced the concept of “cooperative care” further linking the hospitality accommodations with family provided patient care services.
The Oncology Group is well-versed in hotel-hospital accommodation arrangements. They can also work with your team to explore and discuss the cooperative care model, currently used most often with BMT patients.
×